These are turbulent times within healthcare. Since 2007 there have been around 28 major changes to the NHS instigated by governments of all persuasions. In 2010 David Cameron said:
“With the Conservatives there will be no more of the tiresome, meddlesome, top-down re-structures that have dominated the last decade of the NHS.”
Yet his government has been responsible for the biggest and costliest top-down change of all, courtesy of the 2012 Health and Social Care Act. This is not a partisan blog but from many years of working with senior management in the NHS on an interim and consultancy basis I am convinced that meddling from Westminster is the cause of very many of the intractable problems of running an NHS trust. Arguably the best thing any government could do for the NHS is to stop making changes and let the management teams do the jobs for which they were recruited without intolerable pressures.
And let’s face it, running a hospital with 3,000 employees, a budget of £250m and more patient visits than you can shake the proverbial stick at is a hellishly difficult job even without continuous cycles of questionable change.
Don’t get me wrong, some changes have been for the better: waiting times are shorter and quality outcomes in particular areas are improving, notably cancer treatments. But many more have been counterproductive, the result of ill-informed or dogmatic change being thrust upon services when they are already hard-pressed.
Why? Because they force management teams to take their collective eyes off the ball and away from serving the needs of the local demographic. While nobody would argue that spending scarce funds wisely is essential, putting financial targets top of the agenda rather than patient treatment has been the most divisive change of all.
My experience is that board members are already immersed in greater operational detail than in any comparable organisation in the private sector, and often taking gung ho first hand responsibility for crisis management, with the result that NHS Trusts are rarely as proactive or strategic as they should be – the job you would expect the top bods to be doing.
After all, everything will change in 3-5 years, so how can you plan ahead, particularly when crises are overwhelming and there are monthly targets to be met? CEOs and COOs are currently juggling chainsaws more than planning improvements to patient care and nurturing their teams to greater success, and you can hardly blame them for the stress of having to run the show, plan change, break even and deal with a very uncertain future level of demand as CCGs flex their muscles, not to mention penalties levied.
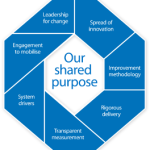
The point is that the Holy Grail must be clarity of vision and sustainable delivery, but fire-fighting is addictive. This gives interim senior managers, the people brought in to fill the ever-widening skills gap and to manage the endless transformational changes, a challenge and a dilemma. We CAN make a difference to how well Trusts adapt to change, by virtue of experience elsewhere and spotting the opportunities that staff are too close to see.
After all, we are brought in to do a specific job, possibly to fill in pending the recruitment of a substantive, to effect a particular change or meet a target, though typically it may be the underlying issues that need to be changed in order to make a difference. Not just tools and techniques embedded (many of which are provided through the IST, for example) or process steps to be re-engineered, but priorities changed and bottlenecks removed.
A week or two of humility and root cause analysis will pay dividends: listening to the frustrations of people throughout the organisation, may well persuade you that there are more urgent priorities which would be a better use of your time, but first you have to get a worthy consensus of opinion and develop a rational case to present to your sponsor. persuade them to allow you time to conduct a feasibility study or maybe a pilot area to deliver the compelling evidence which to back up your argument.
A tough call, given that they will be swamped with irresistible persuasion to pull them in a thousand directions, many conflicting. In some cases it may make you highly unpopular to suggest actions contrary to the current fashion, but if you are offering a professional opinion based on genuine conviction then identifying not only quick wins within your limited time on site but also the strategic changes, the big stuff that will make the greatest difference, is a duty.
You can’t force any client to bite but being persuasive is what the interim game is all about: making people in power sit up and take notice, and then to do the stuff that keeps us in gainful employment: making a REAL difference.
Just stumbled across this, interesting and rings true in a lot of what I currently experience in a leadership development year within the NHS.